www.drjwv.com
Newsletter:
Written by: Jeff Vidt, DVM
Volume 3, Issue 3
September 1999
Familial Shar-Pei Fever (FSF) has been reeconginzed problem in the Chinese Shar-Pei breed since the early 1980's.
Research has given us much information concerning the hereditary aspects of the disease and some of teh pathophysiology of
the condition, but unfortunately, no blood test to diagnose the disease. Recent advances in molecular genetics have
demonstrated that FSF is not the same disease as Familial Mediterranean Fever in man, even though the symptoms are very
similar. With advances in melecular biology and break throughs in other genetic diseases, it is only a matter of time
before we have enough information to make some headway in the diagnosis of FSF. Until then, what can we do? I think we
have to institute breeding proctivces which will give us the best chance to breed away from the disease. I recommend breeding
for logevity. Even if the dam or sire die of amyloidosis at 10 years of age I can accept that. I would not breed to any line
with FSF and/or amyloidosis in its background. I also would not breed to any dog with FSF, amyloidosis or unexplained kidney disease it its
pedigree. These recommendations require that breeders do their homework and communicate with each other honestly. It requires
breeders to follow up on their puppies and see what's happening to them several years down the line. You know though, breeding good,
healthy, sound dogs have been easy. This issue of the newsletter contains one topic -- a plan of action to diagnose kidney failure in Shar-Pei
at an early stage when treatment has the best chance of success. I hope you find it helpful and informative. If you have any questions about
FSF, amyloidosis and/or kidney failure please don't hesitate to call the office or schedule and appointment.
 Plan of Action for Amyloidosis
Plan of Action for Amyloidosis
This article by Dr. Vidt
presents a plan to monitor Shar-Pei with the goal of uncovering renal
amyloidosis as early as possible and then instituting appropriate dietary and
medical intervention. It does contain some technical terms which your
veterinarian may be able to simplify for you. The author urges you to discuss
this article with veterinarian and then both of you can work together in
dealing with this troubling disease.
Renal amyloidosis has hit the
Shar-Pei fancy in recent years and left many of us feeling helpless as we watch
young Shar-Pei sicken and die before our very eyes. We don't have to sit and
take it, but can gather the facts and formulate a plan of action. What I
propose in this paper is based on the information available today about renal
amyloidosis. Currently, there is no test available to help pinpoint Shar-Pei at
risk for developing the condition and due to ethical considerations, information
concerning pedigree analysis is not available to help determine those dogs who
have the condition in their background. What we are left with is to try to
uncover the condition in our dogs as early as possible and to institute steps
to minimize the effects on our dogs and increase longevity. The following plan
has no guarantees and certainly will change as new information becomes
available, but it represents a starting point and a step to build on further.
Keeping a Watchful Eye for the Health of your Shar-Pei
As a Shar-Pei owner you can
do the following simple steps:
- Monitor weight - This
involves weighing your dog at regular intervals using a scale. Do not rely
on eyeball judgements. Too often I see dogs in an advanced state of weight
loss which the owner has just noticed, but which has been going on for
several weeks. Remember, we are trying to uncover this condition at its
earliest point - minor weight loss can indicate early renal amyloidosis.
- Monitor appetite - Daily
fluctuations in appetite do occur, but a change in what is normal for your
dog may indicate early kidney problems.
- Monitor water consumption -
A normal dog consumes approximately 1 oz. of water per pound of body
weight per day. This varies with activity level, season of the year, type
of food being fed (canned vs. dry), etc. I advise measuring water intake
periodically by measuring how much water is put down in the morning and
measuring it again at night. Obviously this will involve a little more
ingenuity on the owner's part when multiple dogs are involved. Increased
water consumption may indicate early kidney failure.
In addition to the above home
monitoring program, I also advise having your veterinarian check a urine sample
every three months on any Shar-Pei over two years of age. The main parameters I
watch in the urine are the urine specific gravity and the urine protein
reading. Urine specific gravity is a measure of the concentration of the urine.
If the kidneys were not functioning at all this reading would be 1.008 - 1.012
(a dilute urine). Normal concentration should be above 1.025 and sually is
greater that 1.045 (a concentrated urine). Ideally the urine sample should be a
morning sample collected after the dog's water bowl has been removed overnight
(remember to close the toilet lid!). By depriving the dog of water overnight we
force the kidneys to concentrate the urine, if they are able to do so.
Inability to concentrate urine indicates that approximately 75% of the kidneys
are non-functional - this is still compatible with life, but treatment needs to be started quickly to preserve the remaining kidney
function.
The other urine test I
heavily rely on is the urine protein level. The stick test routinely run by
veterinarians primarily measures urine albumin levels. An elevated urine
albumin level means that protein is being lost in the urine and correlates with
glomerular damage (the glomerulus is the filtration unit of the kidney and
serves to filter out the waste products of the body). High levels of protein in
the urine indicates significant kidney disease and additional testing needs to
be done to obtain a diagnosis. A new more quantitative microalbuminuria test
is now available for in-hospital use from Heska, the E.R.D.-Screen™ Urine
Test. The “gold standard” for proteinuria is the urine protein/creatinine
ratio (UPC) which is run by all the commercial veterinary laboratories.
It appears that there are
three separate syndromes associated with renal amyloidosis in the Shar-Pei:
- Glomerular - If the amyloid
deposits occur primarily in the glomerulus, we see increased protein
levels in the urine.
- Tubular - If the amyloid
deposits occur in the tubular part of the kidney we see loss of
concentrating ability which manifests as a dilute urine.
- Combination - This occurs
when amyloid is deposited in both the glomeruli and the kidney tubules and
we see increased protein levels in the urine and dilute urine.
The clinical signs and the
routine urine check constitute the first level of diagnostics. If the
urine sample is abnormal and one or more clinical signs are present, then we
immediately proceed to the second level of diagnostics. This level incorporates
the following tests:
- A complete blood count - This includes a packed cell volume, a white blood
cell count, red blood cell count, platelet count, and a white blood cell differential count.
- A health panel - This
includes at least a BUN, creatinine, sodium, potassium, calcium, phosphorous, cholesterol, total protein, albumin, globulin and, glucose. It often includes liver tests and thyroid hormone levels.
- An immune panel - This
should consist of a direct Coomb's test, an anti-nuclear
antibody test (ANA), a Rheumatoid arthritis factor test (RA),
and an LE prep for systemic lupus.
- A urine protein/creatinine
ratio - A value above 1.0 is considered abnormal
and indicates excessive urine protein loss.
- Abdominal radiographs -
Used to evaluate kidney size and shape.
Based on the results of the
first and second level diagnostics the following steps are taken to manage the
patient:
- Diet - A low protein diet
is initiated using Hill's Prescription Diet
K/Dâ or its home-made counterpart. I’m also using the Iams Eukanuba
Veterinary Kidney Diets – Early Stagesâ and Advanced Stagesâ. There are other kidney diets available as well by other pet food
manufacturers.
- Vitamin-mineral
supplementation.
- Ascriptinâ – 1/4 tablet once a day or low dose
aspirin(81mg) ˝-1 tablet daily.
- 1-2 cooked eggs per day -
used in cases where albumin is being lost in the
urine.
- Additional medical therapy
may be instituted using either colchicines tablets or DMSO via injection
or orally. The effectiveness of both these drugs in the prevention and
treatment of renal amyloidosis in the dog has yet to be substantiated, but
their use is justified given the grave prognosis of this condition in the
Shar-Pei. Colchicine is a human anti-gout medication whose mode of action
is largely unknown. It appears to prevent the formation of amyloid in the
laboratory, but whether this occurs in the living animal is not known.
Dimethyl sulfoxide (DMSO) is another drug whose mode of action is unknown,
but has demonstrated the property of dissolving amyloid in the laboratory.
Again, whether this action occurs in the living animal is unknown. The
dosages are as follows:
A.
Colchicine - this dose can be
obtained from Dr. Linda Tintle or myself (see the July/August 1992 issue of The
Barker).
B.
DMSO - numerous dosages are in the
veterinary literature. Your veterinarian should refer to an excellent article
on renal amyloidosis by Dr. DiBartola in Current Veterinary Therapy XI.
[IMPORTANT!
- DMSO imparts an odor to the breath and skin of the patient.]
Again,
the effectiveness of these drugs in the treatment of amyloidosis has not been
proven in clinical studies and hence, they should be regarded as experimental
drugs for this use. They should be used only under the supervision of your
veterinarian.
- Equally important is the
avoidance of further kidney damage. -
A.
Avoid dehydration- provide plenty
of fresh water daily.
B.
Avoid kidney-damaging drugs such
as aminoglycoside antibiotics, methoxyflurane anesthesia, various
chemotherapeutic agents, sulfonamide antibiotics, etc.
C.
Avoid stress- boarding, traveling,
showing, etc.
Third level diagnostics may be done depending on your
veterinarian or the availability of specialists in your area. Test at the level
may include:
- Coagulation panel -
Increased levels of fibrinogen may indicate
impending
thromboembolism (throwing of blood clots) associated with DIC (Disseminated
Intravascular Coagulation) especially if
associated
with increased cholesterol and decreased albumin levels
(nephrotic
syndrome). This panel should include a platelet count and a measurement of
FDP’s (Fibrin Degradation Products).
- Fractional clearances of
various eletrolytes (sodium, potassium, calcium and phosphorous).
- 24-hour urine protein
excretion.
- Creatinine clearance testing
to evaluate kidney function (glomerular filtration rate – GFR).
- Kidney ultrasound.
- Kidney biopsy.
The kidney biopsy is the definitive
diagnosis of renal amyloidosis and the decision to biopsy should be made early
in the course of the disease for a number of reasons:
- Early on, the animal is a
much better surgical candidate and many complications of renal amyloidosis
such as bleeding tendencies and uremia are not present.
- There is a real danger in
the Shar-Pei to blame every kidney problem on renal amyloidosis and fail
to pursue other causes of kidney disease such as kidney infection,
heartworm disease, and immune-mediated diseases like systemic lupus and
immune-mediated glomerulonephritis.
- The information from an
early kidney biopsy can guide the medical and dietary management of the
case and provide valuable prognostic information.
Almost as important as the
early diagnosis of renal amyloidosis is the continued monitoring of the patient
while on therapy. This allows us not only to monitor and watch for the
progression of the disease, but also to evaluate the various therapeutic
modalities and determine which are effective and which are not. Monitoring at
one to two week intervals initially and then at monthly intervals thereafter is
recommended. I usually repeat a kidney panel and cholesterol level, a CBC, and
a urinalysis including a urine protein/creatinine ratio.
Continued monitoring is also
important in order to pick up the early signs of sequelae to renal amyloidosis
such as:
- Nephrotic syndrome -
characterized by decreased serum albumin, increased serum cholesterol and
increased protein loss in the urine. A serious complication of this
syndrome is thromboembolism ("throwing blood clots"). Your
veterinarian may do a blood fibrinogen level and coagulation panel to
evaluate the blood clotting system. If the fibrinogen level is >300
mg/dl, aspirin therapy is strongly indicated. Another serious complication
of this condition is the development of edema or fluid accumulation in the
abdomen or chest and in the limbs. In this case, the use of diuretics such
as Lasix may be necessary.
- Uremia - or the
accumulation of body waste products which are normally filtered by the
kidneys into the urine. The build-up of these wastes causes clinical signs
such as appetite loss, weight loss, vomiting, diarrhea, depression and
lethargy. More serious effects include anemia (decreased red blood cell
production) and gastrointestinal ulceration. Treatment here may include
intravenous fluid therapy, dietary therapy such as Hill's Science Diet U/Dâ, Iams Eukanuba Veterinary Kidney Diet – Advanced
Stagesâ, phosphate binders such as Amphojelâ, ulcer medication such as Carafateâ and other therapy as deemed necessaryby your
veterinarian. Eventually, uremia will progress and lead to the
death
of the animal. As an aside, current nutritional research indicates that there
is no advantage to instituting dietary protein restriction prior to the onset
of kidney failure. This means that feeding protein-restricted diets prior
to developing laboratory or clinical signs of kidney failure will not prevent
kidney failure.
- Hypertension - The kidneys
are very important in the regulation of blood pressure. It is speculated
that up to 80% of the dogs in kidney failure have significant hypertension
as a consequence. The use of indirect blood pressure monitoring in animals
has recently become available to the veterinarian and hopefully will lead
to more advances in this area. Your veterinarian may wish to institute
therapy using vasodilators and/ or diuretic medication.
- 4.Disseminated
Intravascular Coagulation (DIC)– The body’s coagulation system is in a
fine state of balance between forming blood clots and dissolving them.
When this balance is disrupted coagulation factors are used up before they
can be replaced and out of control bleeding is the result. This condition
is associated with high mortality and is a poor prognostic factor.
Treatment is not very effective.
- Streptococcal Toxic Shock
Syndrome (STSS) –This is an unusual complication which results in areas of
skin death leading to skin sloughing almost like a burn. The condition
seems to be caused by toxins produced by Streptococcus canis and is
rapidly fatal sometimes in spite of treatment.
It should be mentioned here
that DIC and STSS are also complications following episodes of Familial
Shar-Pei Fever (FSF). FSF appears to be a potential trigger for the Systemic
Inflammatory Response Syndrome (SIRS) which can stimulate the development of
DIC and STSS. Ultimately, these end up in the development of Multiple Organ
Dysfunction Syndrome (MODS) if early and aggressive treatment is not
initiated. The bottom line is that no episode of FSF should be treated
lightly. I recommend that my clients call me with each FSF attack and
certainly bring the dog in if the episode is not responding to aspirin, is
lasting longer than usual, they notice any usual symptoms or the fever is very
elevated.
To what extent early
diagnosis and monitoring contributes to the longevity and quality of life of
renal amyloidosis patients is hard to quantify at this time. My feeling is that
it is possible to slow the progression of the condition and improve the short-term
prognosis for these patients. We can probably add several months to their life
span. It's expensive and requires diligence and hard work on the part of both the
owner and their veterinarian, but the reward is some extra time with a close
friend.
Chronic Renal Failure
Treatment
Any or all of the following
therapeutic agents may be used in the treatment of chronic renal failure in
Shar-Pei. The definitive treatment of your dog will depend on decisions made
with your veterinarian. Dosages are based on my experience and may be adjusted
by your veterinarian based on their experience or on more recent dosage
information.
- Fluid therapy – in-hospital
treatment typically involves intravenous administration. Home care may
involve subcutaneous administration. May add B vitamins to stimulate
appetite and replace water-soluble B vitamins. Rate is usually 2-3 times
maintenance.
- Histamine H2-receptor
antagonists to inhibit stomach acid secretion. These include Tagamet HB®,
Pepcid® and Zantac® tablets.
- famotidine (Pepcid AC®)
0.5 mg/kg sid-bid 10 mg tablet
- ranitidine (Zantac®)
2mg/kg tid 75,150, 300 mg tablets
- nizatidine (Axid®) 5 mg/kg
sid 150,300mg capsules
- cimetidine (Tagamet HB®)
10mg/kg bid 100, 150, 200, 300 mg tablets
- Aspirin 81mg tablets – ˝ -
1 tablet once a day for hypercoagulability problems.
- Phosphate binders –
typically aluminum hydroxide agents such as Basaljel®, Amphojel®, Maalox®
and others. Average Shar-Pei would be dosed at 200mg three times a day.
- Aluminum hydroxide 30-90
mg/kg/day
- Aluminum carbonate 30-90
mg/kg/day
- Aluminum oxide 30-90
mg/kg/day
- Calcium acetate 60-90
mg/kg/day
- Calcium carbonate 90-150
mg/kg/day
Another agent is sevelamer (Renagel®) dosed at 30-135 mg/kg/day divided given intact with
meals. This drug does not promote hypercalcemia or absorption of aluminum. Should monitor clotting ability when used in dogs (PT).
A
new veterinary product is Epakitin® available from Vetoquinol which contains
chitosan from shellfish to bind phosphorus. An average Shar-Pei would receive
3 measuring spoons twice a day with food.
- Metoclopramide (Reglan®),
an anti-emetic at 5-10mg three times a day for vomiting. Zofran®
(ondansetron) 0.5-1.0mg/kg 30 minutes before food. Dansetron mesylate
(Anzemet®) is an injectable anti-emetic which is given once a day at
0.3mg/kg.
- Pet Tabs® (vitamins) 1
tablet twice a day.
- 3V Caps® (large breed) 1
capsule once a day – a fatty acid supplement as an anti-inflammatory agent
for the kidneys.
- omega-3 FAs promote kidney
function
- 200 – 250 total
omega-3 FAs/kg/day
- Food = 1-2% total omega-3
FAs
- N-6:N-3 ratio = 2:1
- Colchicine 0.6 mg twice a
day – amyloidosis.
- Human recombinant
erythropoietin (Epogen®, Procrit®) for nonregenerative anemia (low red blood
cell count) associated with chronic renal failure. Start with 100U/kg
subcutaneous injection 3 times a week until PCV is between 37-45% then
decrease schedule to one injection a week. MUST monitor PCV and
serum iron levels. Dogs can develop antibodies to this drug. DO NOT
USE IN DOGS WITH HIGH BLOOD PRESSURE! We want to delay the use of
human EPO due to the risk of antibody production against the hormone (22%)
and the potential of more serious possible cross antibody attack against
the patients’ bone marrow – bone marrow aplasia.
- Enalapril (Enacard®,
Vasotec®) 10 mg tablets ˝-1 tablet once a day for protein-losing
glomerulopathy. Benazepril (Lotensin®) 1 tablet sid 5mg tablet
- Prescription Kidney Diet –
generally low protein and low phosphorous. Hill’s K/D or U/D Diet®, Iams Eukanuba
Veterinary Diets Nutritional Kidney Formula Early Stages or Advanced
Stages Diet®, Purina CNN Kidney Diet®, others. THE MOST IMPORTANT GOAL
IS TO KEEP THE PATIENT EATING – THERE IS NO POINT IN STARVING THE PATIENT
TO USE THE CORRECT DIET!! Feed smaller meals more often – more likely to
hit the dog when they feel like eating.
- Appetite stimulants such as
cyproheptadine (Periactin®) at 5-20mg one to two times a day and
mirtazapine. Propofol at 1mg/kg IV stimulates appetite within 15 minutes.
B vitamins via injection or added to subcutaneous fluids may stimulate
appetite also.
- Proton pump inhibitors --
Prilosec® (omeprazole) 20 mg/dog sid (0.7 mg/kg) 20mg capsule.
- Ulcer adherent complex --
Carafate® (sucralfate) 0.5-1.0gm/dog bid-tid 1 gm tablets.
- Sodium bicarbonate 650 mg
tablets -- 2 tablets tid based on base excess. Try
to maintain plasma HCO3 concentration at 15 mEq/l or greater.
- Ferrous gluconate 242mg
tablet – ˝ tablet sid (see discussion under EPO).
- A new veterinary product
called Azodyl® available from Vetoquinol. It relies on a process called
“enteric dialysis” which utilizes bacteria to fix nitrogen in the colon.
This reduces uremic toxins. The dose for an average size Shar-Pei is 2
capsules in the AM and 1 capsule in the PM.
- Calcitriol – when serum
phosphorus concentration ≤ 6 mg/dl. Initial dose is 2.5ng/kg/day.
May increase calcitriol doses about 0.75-1.0ng/kg to a maximum dose of
5ng/kg. Treatment endpoint is to normalize serum PTH levels without
inducing hypercalcemia.
- Amlodipine besylate
(Lotensin®) is a calcium channel blocker used in treating hypertension.
Start dosing at 0.1mg/kg orally b.i.d. and up-titrate weekly while
monitoring blood pressure.
- ACE (Angiotensin I
Converting Enzyme) AT1 receptor antagonists – irbesartan (Avapro®)
5-30mg/kg once a day, telimsartan(Micardis®) 0.1-1.0mg/kg once a day.
Lastly, when the end does
come, consider allowing your veterinarian to do an autopsy on your dog.
Especially important is the evaluation of the kidneys through histopathology.
We must verify cases of renal amyloidosis or other causes of kidney failure if
we are to make headway in correcting this condition through breeding. Results
can be sent to Dr. Linda Tintle, Wurstboro Veterinary Clinic, PC, 251 Sullivan
Street, P.O. Box 906, Wurtsboro, New York, 12790.
I currently maintain a web
presence at www.drjwv.com. My hope is to update this site
periodically as new information becomes available. This site represents my own
opinions based on reading the veterinary literature and in no way reflects the
opinions of the CSPCA, Inc. or anyone else.
The Officers and Board of
Directors of the Chinese Shar-Pei Club of America supports research for
Familial Shar-Pei Fever and amyloidosis. Donations can be sent to the CSPCA
Charitable Trust, Lee Arnold, Chairman, P.O. Box 7007, Bedminster, NJ 07921.
All donations will be
acknowledged in future issues of The Barker.
Many of us have felt the pain
and loss of a wonderful Chinese Shar-Pei. Let us feel the joy in helping find
solutions.
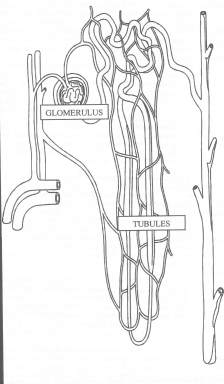
Kidney Unit = The Nephron
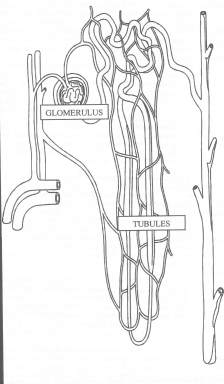 The kidneys consist of millions of nephrons in each kidney. A nephron has a filtration unit called teh glomerulus.
Here there is intimate contact between blood vessels and the kidney cells which allows the exchange of waste products or protein
metabolism from the blood to the urine. We routinely measure some of these waste products in the blood called the BUN and
the Creatinie. From the glomerulus, the urine proceeds to the kidney tubules. The cells lining the tubules
reabsorb some materials in the urine which the body wants to save such as glucose, albumin, etc. and also adjust the
electrolyte levels of sodium, potassium and chloride. This process is reflected in the urine specific gravity.
In the human 100 liters of water pass through the glomerulus in a day, but only 1 liter of water is eliminated in the urine.
The kidny also helps in the control of blood pressure via ther regulation of sodium and water levels in the body.
Lastly, the kidney stimulates the production of red blood cells through a hormone called erythropoietin.
By evaluating the levels of BUN, creatinine, sodium, potassium, chloride and red blood cell percentage along with an overnight water
deprivation urine sample we can get a pretty good idea of how the kidneys are functioning. Actually, the blood
changes in kidney disease represent a later stage or kidney failure than can be dtected in the urine.
When approximately 75% of the kidney is not functioning we see loss of the concentrating ability of the kidney which is
reflected in a dilute urine. This may be noticed clinically as increased water consumption and increased urination
(both amount and frequency). Blood changes don't occur until about 80-85% of the kidney is non-fuctional. By evaluating urine samples
after restricting water overnight we can monitor Shar-Pei for the development and progression of kidney failure. This is the
basis of my recommendation to check urine samples every three months in this breed.
The kidneys consist of millions of nephrons in each kidney. A nephron has a filtration unit called teh glomerulus.
Here there is intimate contact between blood vessels and the kidney cells which allows the exchange of waste products or protein
metabolism from the blood to the urine. We routinely measure some of these waste products in the blood called the BUN and
the Creatinie. From the glomerulus, the urine proceeds to the kidney tubules. The cells lining the tubules
reabsorb some materials in the urine which the body wants to save such as glucose, albumin, etc. and also adjust the
electrolyte levels of sodium, potassium and chloride. This process is reflected in the urine specific gravity.
In the human 100 liters of water pass through the glomerulus in a day, but only 1 liter of water is eliminated in the urine.
The kidny also helps in the control of blood pressure via ther regulation of sodium and water levels in the body.
Lastly, the kidney stimulates the production of red blood cells through a hormone called erythropoietin.
By evaluating the levels of BUN, creatinine, sodium, potassium, chloride and red blood cell percentage along with an overnight water
deprivation urine sample we can get a pretty good idea of how the kidneys are functioning. Actually, the blood
changes in kidney disease represent a later stage or kidney failure than can be dtected in the urine.
When approximately 75% of the kidney is not functioning we see loss of the concentrating ability of the kidney which is
reflected in a dilute urine. This may be noticed clinically as increased water consumption and increased urination
(both amount and frequency). Blood changes don't occur until about 80-85% of the kidney is non-fuctional. By evaluating urine samples
after restricting water overnight we can monitor Shar-Pei for the development and progression of kidney failure. This is the
basis of my recommendation to check urine samples every three months in this breed.
 Plan of Action for Amyloidosis
Plan of Action for Amyloidosis Plan of Action for Amyloidosis
Plan of Action for Amyloidosis
 The kidneys consist of millions of nephrons in each kidney. A nephron has a filtration unit called teh glomerulus.
Here there is intimate contact between blood vessels and the kidney cells which allows the exchange of waste products or protein
metabolism from the blood to the urine. We routinely measure some of these waste products in the blood called the BUN and
the Creatinie. From the glomerulus, the urine proceeds to the kidney tubules. The cells lining the tubules
reabsorb some materials in the urine which the body wants to save such as glucose, albumin, etc. and also adjust the
electrolyte levels of sodium, potassium and chloride. This process is reflected in the urine specific gravity.
In the human 100 liters of water pass through the glomerulus in a day, but only 1 liter of water is eliminated in the urine.
The kidny also helps in the control of blood pressure via ther regulation of sodium and water levels in the body.
Lastly, the kidney stimulates the production of red blood cells through a hormone called erythropoietin.
By evaluating the levels of BUN, creatinine, sodium, potassium, chloride and red blood cell percentage along with an overnight water
deprivation urine sample we can get a pretty good idea of how the kidneys are functioning. Actually, the blood
changes in kidney disease represent a later stage or kidney failure than can be dtected in the urine.
When approximately 75% of the kidney is not functioning we see loss of the concentrating ability of the kidney which is
reflected in a dilute urine. This may be noticed clinically as increased water consumption and increased urination
(both amount and frequency). Blood changes don't occur until about 80-85% of the kidney is non-fuctional. By evaluating urine samples
after restricting water overnight we can monitor Shar-Pei for the development and progression of kidney failure. This is the
basis of my recommendation to check urine samples every three months in this breed.
The kidneys consist of millions of nephrons in each kidney. A nephron has a filtration unit called teh glomerulus.
Here there is intimate contact between blood vessels and the kidney cells which allows the exchange of waste products or protein
metabolism from the blood to the urine. We routinely measure some of these waste products in the blood called the BUN and
the Creatinie. From the glomerulus, the urine proceeds to the kidney tubules. The cells lining the tubules
reabsorb some materials in the urine which the body wants to save such as glucose, albumin, etc. and also adjust the
electrolyte levels of sodium, potassium and chloride. This process is reflected in the urine specific gravity.
In the human 100 liters of water pass through the glomerulus in a day, but only 1 liter of water is eliminated in the urine.
The kidny also helps in the control of blood pressure via ther regulation of sodium and water levels in the body.
Lastly, the kidney stimulates the production of red blood cells through a hormone called erythropoietin.
By evaluating the levels of BUN, creatinine, sodium, potassium, chloride and red blood cell percentage along with an overnight water
deprivation urine sample we can get a pretty good idea of how the kidneys are functioning. Actually, the blood
changes in kidney disease represent a later stage or kidney failure than can be dtected in the urine.
When approximately 75% of the kidney is not functioning we see loss of the concentrating ability of the kidney which is
reflected in a dilute urine. This may be noticed clinically as increased water consumption and increased urination
(both amount and frequency). Blood changes don't occur until about 80-85% of the kidney is non-fuctional. By evaluating urine samples
after restricting water overnight we can monitor Shar-Pei for the development and progression of kidney failure. This is the
basis of my recommendation to check urine samples every three months in this breed.