www.drjwv.com
Newsletter:
Written by: Jeff Vidt, DVM
Volume 4, Issue 1
January 2000
Greetings
I hope everyone had a happy and safe holiday season and are ready to begin the
new millennium with energy. I'm taking some time in this column to thank you,
my Shar-Pei clients, for your continued support over the years. Many of you
started with me at LaGrange Park in 1983 and many have just been with me over
the last few weeks, but I want you to know that I value each and every one of
you. And of course that applies equally to your Pei. This past year has been a
tough one for many of you -- we've lost some of our oldest Shar-Pei this year.
I've also had the joy and hope as many of you brought in new puppies for their
first visit -- that's always refreshing!
Many of you have adopted rescue dogs from RASP and shelters this year and I
commend you for that undertaking. It can be a difficult initial adjustment period,
but these rescue dogs have so much love and devotion to give. I know you will not
be disappointed. your efforts will be rewarded. I've had the privilege of
fostering at least 10 dogs myself and the clinic has had several dogs boarding
for weeks at a time also. My staff has been very helpful in that regard.
As we start this next millennium, veterinary medicine faces many new challenges.
Corporate veterinary medicine, on-line prescription services, newer drugs and
advanced technology all bid fro the client dollar. I urge you to remember loyalty,
courtesy, kindness, compassion and cooperation. Together we can continue to
provide quality veterinary health care and help our dogs have a good quality
life for as long as we have them.
 Again, best wishes for a happy, healthy year 2000 from all of us at the Downers
Grove Animal Medical Clinic to you and your Shar-Pei.
Again, best wishes for a happy, healthy year 2000 from all of us at the Downers
Grove Animal Medical Clinic to you and your Shar-Pei.
Jeff Vidt, DVM
 Masticatory Myositis
Masticatory Myositis
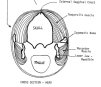
Masticatory mysositis appears to be a breed problem in the Chinese
Shar-Pei. While I'm hesitant to say it's an inherited condition I have
seen it in lines and in litters of affected individuals. This condition
used to be described as two separate disorders: (1)eosinophilic myositis
and (2) atrophic myositis. It is currently felt that these are
manifestations of the same disease now called masticatory myositis.
This is an inflammatory muscle disease, most likely immune-mediated,
involving the muscles of mastication - these muscles are used to grind
and chew food prior to swallowing. Five muscle groups in the dog are
involved in the process of mastication - four muscles are responsible
for closing the mouth and one with opening the mouth. The
tempoallis muscles and the masseter muscles are primarily the muscles
used to powerfully close the jaws and are espacially well developed in
Shar-Pei (Figs. 1 and 2).
Bear in mind that these muscles must also relax in order for the mouth to open.
Since these two muscles are the largest muscles which close the jaw, when they
become involved in masticatory myositis, the primary clinical sign is trouble in
opening the jaws.
Masticatory myositis can be divided into an acute and chronic
form. It must be remembered that one acute attack can lead immediately into
the chronic form of the disease, although, more often than not, multiple,
recurrent acute attacks are necessary. Symptoms of the acute form
involve the the swollen, firm and painful temporalis and masseter muscles.
The dog's head often appears swollen and larger than normal. The dog will
be reluctant or unable to open his mouth. Opening the mouth more than 1 inch
or so elicits an extremely painful response. This results in difficulty in
eating and often the owner notices increased drooling as well. This swelling
may even cause exophthalmia or the eyes to "bug out". Usually a fever is
present and the lymph nodes in the head and neck region are enlarged.
The tonsils are often enlarged as well, but it is difficult to visualize them
due to the inability to open the mouth. The patient is often depressed and
may resent palpation of the head musculature.
Laboratory findings are variable, but very often are normal. The white
blood cell count may be elevated and often there is an increase in eosinophils
(a type of white blood cell often seen with inflammation). Most often there
is a dramatic increase in a skeletal muscle enzyme known as creatine kinase
or creatine phosphokinase (CPK-MM). Smaller amounts of this enzyme
are also located in the brain (CPK-BB) and in the heart muscle (CPK-MB). This
enzyme has a short life span in the serum and is most often elevated in the acute form
of the disease due to the magnitude of muscle damage and because the owner usually
presents the dog while the disease is present. CPK may not be part of the normal
serum enzyme panel your veterinarian uses and may have to be requested separately.
Your vet should also request the CPK enzyme be reported in terms of the various
isoenzymes (heart, brain and skeletal muscles).
The chronic form usually is evident when the dog's head appears "sunken",
especially the top of the head. Sever and recurrent muscle damage leads to scar
tissue formation and atrophy or shrinking of the muscle. This scar tissue is non-functional
and these dogs often cannot open their mouths more than 1/2-1 inch. The dog's
head often appears "skull-like" with a prominent external sagittal crest
(the bony ridge on top of the head) and the eyes are sometimes enophthalmic or
sunken due to loss of the muscle mass behind them (fig.3). In the chronic
form, laboratory findings are often normal. The CPK-MM is usually normal due to the
fact that there is little muscle left to produce the enzyme. The dogs are normal
otherwise and non-painful, although the mouth cannot be opened.
The cause of masticatory myositis is uncertain, but is thought to be
immune-mediated because:
- The type of cellular infiltrate in the affected muscles.
- The disease is responsive to immunosuppressive doses of corticosteroids.
- In some cases, autoantibodies are present, fixed to the unique
muscles fibers present in the muscles of mastication (Type II M fibers)
and the presence of anti-Type II M antibodies in the serum of some
dogs with the disease. These antibodies may play a role in the immune
system attack on these muscle fibers.
Definitive diagnosis of this condition is based on muscle biopsy --
usually of the temporalis and/or masseter muscles. Also a 2M Antibody
test is available which can be done utilizing a serum sample -- this must
be done before therapy is initiated! This test available from:
Comparative Neuromuscular Laboratory
Basic Science Building, Room 1057
University of California, San Diego
La Jolla, CA 92093-0612
Phone: (858) 534-1537
Fax: (858) 534-7319
Treatment invariably involves the use of corticosteroids at high (immunosuppressive)
doses. Prednisolone is usually preferred. In the acute form, there is usually rapid
clinical improvement. The dose is subsequently reduced gradually and in some dogs,
prone to relapses, must be maintained on continuous alternate day therapy. In the
chronic form the prognosis is much more guarded. Surgery is usually done to allow
some return of jaw function. Often the insertion of the temporal muscle on the lower
jaw is surgically incised and released. This may free up the jaw enough for the dog
to be functional.
Fortunately, this is not a common disease, but one that veterinarians and owners
need to be aware of.
Eploratory Laparotomy
 The exploratory laparotomy is an abdominal surgery whose purpose is to search
for disease in the abdominal organs. Often, diagnostic tests such as the physical
examination, blood testing, urinalysis, radiographs, even ultrasounds are unable
to diagnose some disease problems especially those involving the gastrointestinal
tract. Many times the best thing to do is to surgically open the abdomen and look
at the organs for abnormalities. Not only can the organs be visualized, but biopsy
samples can be obtained, if indicated. Often, even a cure can be secured if we are
dealing with a surgically correctable problem such as an intestinal foreign object,
some tumors, etc. The key is to do the surgery early while the dog is still in
reasonably good shape. While it seems like a major undertaking, with today's newer
anesthetic agents and better equipment, the exploratory laparotomy is a valuable
and very cost-effective diagnostic procedure.
The exploratory laparotomy is an abdominal surgery whose purpose is to search
for disease in the abdominal organs. Often, diagnostic tests such as the physical
examination, blood testing, urinalysis, radiographs, even ultrasounds are unable
to diagnose some disease problems especially those involving the gastrointestinal
tract. Many times the best thing to do is to surgically open the abdomen and look
at the organs for abnormalities. Not only can the organs be visualized, but biopsy
samples can be obtained, if indicated. Often, even a cure can be secured if we are
dealing with a surgically correctable problem such as an intestinal foreign object,
some tumors, etc. The key is to do the surgery early while the dog is still in
reasonably good shape. While it seems like a major undertaking, with today's newer
anesthetic agents and better equipment, the exploratory laparotomy is a valuable
and very cost-effective diagnostic procedure.
What is Pain?
 First we need to define and understand pain.
First we need to define and understand pain.
- In its simplest form pain is a perception. A noxious stimulus has to be
recongnized by the animal. This stimulus is usually of such intensity that there
is a behavioral or physiological change that occurs -- the animal reacts to the
pain. The intensity of the pain often is indicated by the magnitude of the pet's
response.
- Pain, if left untreated, results in mental distress and anxiety which we call
suffering. It can also result in physical injury as the animal attempts to alleviate
the pain.
- There is "good" pain and "bad" pain. "Good" pain has a protective function
under normal circumstances. Pain caused by excessive heat teaches the animal
to avoid physical harm due to fire. This type of pain can be avoided or escaped
from. "Bad" pain is pain associated with trauma, surgery or disease. This type
of pain cannot be avoided by a behavioral response by the pet and needs to be
medically managed. "Bad" pain results in abnormal physical and psychological
stress on the animal.
- We also need to consider "acute" pain versus "chronic" pain. Acute pain is
associated with trauma, burns, post-surgery, and orthopedic/musculoskeletal injuries.
It will eventually resolve. On the other hand chronic pain is primarily associated
with cancer, chronic long-term disease and arthritis. Chronic pain will not go
away -- it is a long-term problem and has to be medically managed to make the
animal comfortable.
Drug Therapy in Pain Management
In veterinary medicine we are limited in the number of oral pain medications we
can use for control of pain.
- NONSTEROIDAL ANTI-INFLAMMATORY DRUGS or NSAIDs include two distinct
subclasses: the carboxylic acids and the enolic acids. The carboxylic acid group
can be further subdivided into the salicylates, proprionic acid derivatives and
fenamic acids. ASPIRIN, a salicylate, is a very common, mild analgesic
(pain relieving) medication. It is useful for the low-grade pain of arthritis
and minor trauma. It is available over-the-counter and is inexpensive. IT IS
TOXIC IN CATS! The most common side-effects are gastrointestinal irritation.
NAPROXEN (Aleve®), IBUPROFEN (Motrin®, Nuprin®) and
KETOPROFEN (Orudis®) are proprionic acid derivatives. These can NOT be
used in dogs or cats as they have a higher incidence of moderate to sever side-effects
such as gastrointestinal tract hemorrhage, ulceration and perforation and kidney
failure. They are not used in veterinary medicine. NSAIDs reduce pain by inhibiting
the inflammatory response that increases sensitivity to pain. They also act centrally
in the spinal cord as well. These agents are useful for soft tissue pain. Two
new veterinary NSAIDs are now available, RIMADYL® (carprofen) and
ETOGESIC® (etodolac). These drugs have greatly increased our effectiveness
in managing the pain of arthritis and mild post-operative pain. Side-effects have
been minimal. Again, these agents are not used in cats.
- NARCOTICS(OPIOIDS) are potent and specific analgesic drugs. Morphine
is the oldest and most well-know of these agents. Opioids interact with specific
receptors in the spinal cord to inhibit pain signal transmission to the brain.
They also act in the brain to block the perception of pain. The most common agent
used in veterinary medicine is TORBUTROL® (butorphenol). This is available
in tablet form and we often dispense a 3-5 day supply as a post-operative analgsic.
During surgery we usually give this drug as an injection to begin the pain management
protocol. This drug is a controlled substance which requires record keeping and is
more expensive than aspirin -- it is also a much more effective pain relieving medication.
Other opioid drugs are not that useful because they can't be given orally for
at home care. SEDATIVES ARE TRANQUILIZERS ARE NOT ANALGESIC, although they are
often used in conjunction with pain medications.
WHAT DOES PAIN LOOK LIKE IN OUR PETS?
One of the main problems associated with pain management in animals is that our
patients can't communicate with us verbally. We have to watch for signs of pain
through behavioral changes such as:
- Decreased appetite
- Decreased activity
- Licking, chewing or scratching at a specific body site.
- Guarding or splinting of the affected area.
- Restlessness, not sleeping, pacing.
- Dilated pupils and anxious wide-eyed expression.
- Rapid breathing, panting.
- Increased heart rate.
- Sensitivity to touching a body part or area.
 Masticatory Myositis
Masticatory Myositis Again, best wishes for a happy, healthy year 2000 from all of us at the Downers
Grove Animal Medical Clinic to you and your Shar-Pei.
Again, best wishes for a happy, healthy year 2000 from all of us at the Downers
Grove Animal Medical Clinic to you and your Shar-Pei. Masticatory Myositis
Masticatory Myositis

 The exploratory laparotomy is an abdominal surgery whose purpose is to search
for disease in the abdominal organs. Often, diagnostic tests such as the physical
examination, blood testing, urinalysis, radiographs, even ultrasounds are unable
to diagnose some disease problems especially those involving the gastrointestinal
tract. Many times the best thing to do is to surgically open the abdomen and look
at the organs for abnormalities. Not only can the organs be visualized, but biopsy
samples can be obtained, if indicated. Often, even a cure can be secured if we are
dealing with a surgically correctable problem such as an intestinal foreign object,
some tumors, etc. The key is to do the surgery early while the dog is still in
reasonably good shape. While it seems like a major undertaking, with today's newer
anesthetic agents and better equipment, the exploratory laparotomy is a valuable
and very cost-effective diagnostic procedure.
The exploratory laparotomy is an abdominal surgery whose purpose is to search
for disease in the abdominal organs. Often, diagnostic tests such as the physical
examination, blood testing, urinalysis, radiographs, even ultrasounds are unable
to diagnose some disease problems especially those involving the gastrointestinal
tract. Many times the best thing to do is to surgically open the abdomen and look
at the organs for abnormalities. Not only can the organs be visualized, but biopsy
samples can be obtained, if indicated. Often, even a cure can be secured if we are
dealing with a surgically correctable problem such as an intestinal foreign object,
some tumors, etc. The key is to do the surgery early while the dog is still in
reasonably good shape. While it seems like a major undertaking, with today's newer
anesthetic agents and better equipment, the exploratory laparotomy is a valuable
and very cost-effective diagnostic procedure.
 First we need to define and understand pain.
First we need to define and understand pain.